Developing non-hormonal, reversible contraception to provide options outside of vasectomy.
Male Contraceptive Initiative is dedicated to supporting the development of new, non-hormonal, reversible male birth control options. We provide funding and advocacy to researchers working diligently on this groundbreaking area of reproductive health.
Explore Your Options
Join us in advocating for expanded reproductive choices for men!
Explore Your Options
- Current Contraceptives: Learn about the limited options available for sperm-producers today.
- The Future of Male Contraception: Discover the promising research and development efforts underway to bring innovative new methods to market.
Join us in advocating for expanded reproductive choices for men!
Expanding Reproductive Choices: The Importance of Male Birth Control
Empowering Couples: The Power of Male Contraception
Male Contraceptive Initiative is dedicated to expanding the range of contraceptive options available to men. By supporting the development of new, non-hormonal, reversible methods, we aim to:
Male Contraceptive Initiative is dedicated to expanding the range of contraceptive options available to men. By supporting the development of new, non-hormonal, reversible methods, we aim to:
- Empower men: Provide men with greater control over their reproductive health.
- Strengthen relationships: Foster stronger, healthier relationships based on equality and mutual understanding.
- Promote reproductive autonomy: Empower individuals and couples to make informed choices about family planning.
Traditional Male Contraceptive Options
Vasectomy
|
Vasectomy is a safe and effective form of permanent male birth control. It involves a simple surgical procedure that prevents sperm from reaching the urethra, thus preventing fertilization.
Key Points:
If you're considering vasectomy, it's important to consult with a qualified healthcare professional to discuss the procedure, potential risks, and benefits, as well as any concerns you may have. |
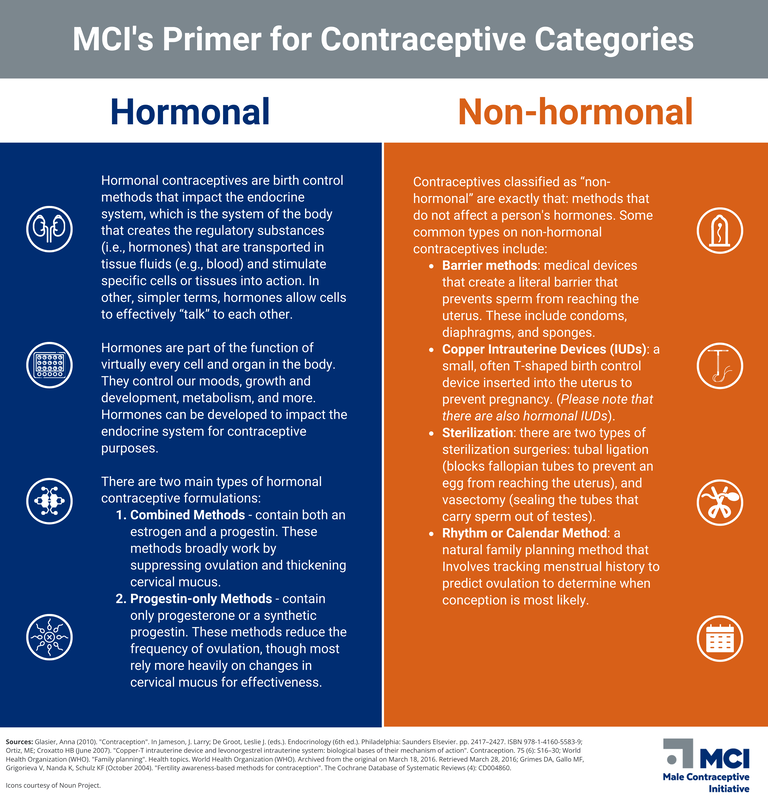
"Existing Contraceptive Methods" Infographic
|
Condoms
|
Condoms are the only reversible, non-hormonal form of male contraception that also offers protection against sexually transmitted infections (STIs). They are barrier devices used during sexual intercourse to prevent pregnancy and STIs.
Key Benefits of Condoms:
|
MCI's "Nuts & Bolts: 10 Facts About Vasectomy" Animated Video
|
How to Use Condoms:
Where to Obtain Condoms: Condoms are available over-the-counter at drugstores, supermarkets, and family planning clinics. Public health organizations often distribute condoms for free to promote safer sex practices.
Remember: Consistent and correct use of condoms is crucial for achieving the desired level of protection against pregnancy and STIs.
- Proper application: Correct application and removal techniques are essential to prevent tears or slippage.
- Consistency: Use a condom during every act of intercourse for maximum effectiveness.
Where to Obtain Condoms: Condoms are available over-the-counter at drugstores, supermarkets, and family planning clinics. Public health organizations often distribute condoms for free to promote safer sex practices.
Remember: Consistent and correct use of condoms is crucial for achieving the desired level of protection against pregnancy and STIs.
Challenges & Limitations
Vasectomy
|
While vasectomy offers reliable and permanent contraception, it's important to carefully consider the potential emotional and psychological consequences of this decision. Some individuals may experience feelings of regret or loss of reproductive options if their life circumstances change.
Misconceptions about vasectomy can also pose challenges. It's crucial to dispel myths and provide accurate information about the procedure, its impact on masculinity and sexual performance, and the potential for reversal. |
MCI's "Nuts & Bolts: Vasectomy" Animated Short
|
Condoms
|
MCI's "Nuts & Bolts: Condoms" Animated Short
|
Condoms are widely accessible and effective, but they do have limitations:
|
Informed Decision-making
It's important to weigh the benefits and drawbacks of each contraceptive option and make an informed decision based on individual needs and preferences. Consulting with a healthcare provider can help you understand the risks and benefits of vasectomy and condoms and choose the best option for you.
Expanding Reproductive Choices: The Need for Alternative Male Contraception
The landscape of reproductive health is evolving, and there is a growing demand for a wider range of male contraceptive options beyond vasectomy and condoms. These traditional methods have limitations that highlight the need for more flexible and accessible options for diverse populations.
The Benefits of Expanding Male Contraception:
By investing in the development of alternative male contraceptives, we can create a more equitable and inclusive reproductive health landscape.
The Benefits of Expanding Male Contraception:
- Challenging gender norms: Involving men more directly in family planning can challenge traditional gender roles and promote healthier relationships.
- Empowering couples: Expanding contraceptive choices allows couples to make joint decisions that align with their life stages, relationship dynamics, and desired family size.
- Improving physical and environmental health: Male contraception can contribute to better physical and environmental health outcomes, aligning with Sustainable Development Goals.
- Serving the LGBTQIA+ community: Providing accessible and effective male contraception options is essential for members of the LGBTQIA+ community.
By investing in the development of alternative male contraceptives, we can create a more equitable and inclusive reproductive health landscape.
Non-Hormonal Male Contraception: A Closer Look
Hormonal contraceptives work by influencing the endocrine system, the body's system of hormones that regulate various functions like mood, growth, metabolism, and reproduction. Disruptions to the endocrine system can impact fertility, which is why hormonal contraceptives can be effective.
Non-hormonal contraceptives, on the other hand, do not affect hormones. Common types include:
While non-hormonal methods often have fewer side effects than hormonal ones, some, like withdrawal and the rhythm method, have low effectiveness. It's important to choose a method that aligns with your individual needs and preferences!
Non-hormonal contraceptives, on the other hand, do not affect hormones. Common types include:
- Barrier methods: Condoms, diaphragms, and sponges physically prevent sperm from reaching the uterus.
- Copper IUDs: A small, T-shaped device inserted into the uterus to prevent pregnancy.
- Outercourse: Engaging in sexual acts without vaginal penetration.
- Withdrawal: Removing the penis before ejaculation.
- Sterilization: Permanent procedures like vasectomy for men or tubal ligation for women.
- Rhythm method: Tracking menstrual cycles to predict ovulation and avoid conception.
While non-hormonal methods often have fewer side effects than hormonal ones, some, like withdrawal and the rhythm method, have low effectiveness. It's important to choose a method that aligns with your individual needs and preferences!
Novel Non-Hormonal Contraception: A New Era
The development of non-hormonal contraceptives is revolutionizing the landscape of family planning. These innovative products offer men greater flexibility and choice, similar to hormonal options, without the associated drawbacks.
How Non-Hormonal Contraceptives Work:
How Non-Hormonal Contraceptives Work:
- Targeted approach: Unlike hormonal methods, non-hormonal contraceptives focus on inhibiting specific cellular activities involved in sperm production, transport, or function.
- Reduced side effects: This targeted approach minimizes the risk of "off-target" effects, resulting in fewer or no side effects.
Male Contraceptive Initiative's Focus
At Male Contraceptive Initiative, we're committed to providing men with reliable, safe, and reversible birth control options. Our focus on non-hormonal contraceptives aligns with our vision of reproductive autonomy for all.
Innovative Approaches:
At Male Contraceptive Initiative, we're committed to providing men with reliable, safe, and reversible birth control options. Our focus on non-hormonal contraceptives aligns with our vision of reproductive autonomy for all.
Innovative Approaches:
- Disrupting sperm production: Targeting the process of spermatogenesis.
- Impairing sperm motility: Interfering with the ability of sperm to move.
- Blocking sperm transport: Preventing sperm from reaching the urethra.
- Altering sperm function: Affecting the sperm's ability to fertilize an egg.
These pioneering mechanisms hold immense potential for transforming family planning by offering effective, reversible male contraception without hormonal side effects.
Progress & Research
|
MCI is committed to furthering the research and development of non-hormonal, reversible male contraceptive options, and offer support through scientific granting to a diverse portfolio of researchers. Our grantees work from the basic science all the way through the drug development pipeline to clinical trials to make the next generation of non-hormonal, reversible male birth control a reality.
MCI provides funding and advocacy support for myriad different potential male contraceptives in order to ensure that a robust method mix is in development every step of the way. Through these efforts, we hope to ensure that the individual needs and interests of men and couples are catered to in order to ensure early adoption and continued use of these critically important, yet currently missing, family planning tools. These alternatives to condoms and vasectomy that researchers are working on now, include varied and diverse options. |
"Vasectomy Alternatives & Next Generation Male Contraception" Infographic
|
What are the male birth control research activities MCI is supporting?
The science of male birth control can be a little intimidating if you do not have a background in science. To counter this, we created this section to make the work we are supporting a bit more accessible to the general public.
A single injection that ensures a man cannot cause a pregnancy for years and is completely reversible.
|
Our grantee Contraline has invented a proprietary hydrogel called ADAM™ that is implanted into the vas deferens through a minimally invasive, outpatient procedure.
The hydrogel works by blocking sperm from traveling through the vas deferens. Similar to intrauterine devices (IUDs) for women, Contraline’s contraceptive is designed to last for years and be reversible. MCI’s support will be used by Contraline to prepare for filing with the FDA and initiating first-in-human trials. |
A reversible male birth control that impacts the head of the sperm, preventing it from fertilizing an egg.
|
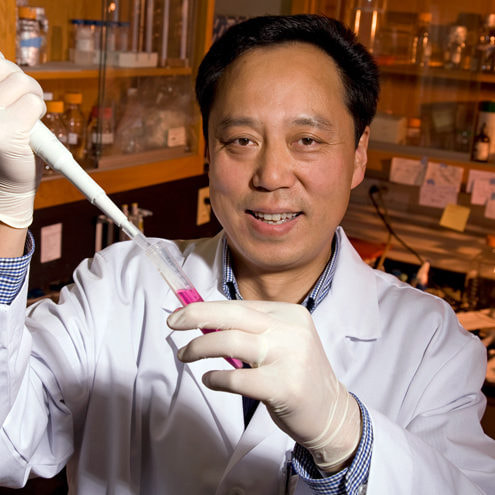
Our grantee Dr. Wei Yan and his team of researchers have developed a new compound derived from a Chinese herb called the Thunder God vine (Tripterygium Wilfordii Hook F).
The compound works by causing the head of sperm to be malformed such that they are not able to connect with and fertilize a female egg. This effect only occurs while the compound is consumed, and normal function is fully restored after discontinuing use. MCI’s support allowed Dr. Yan and his team to explore the effects of the compound and publish their results. Because of MCI’s grant, our sister organization Contraceptive Accelerator Network is performing nonclinical studies on Triptonide that advance it towards human studies. |
|
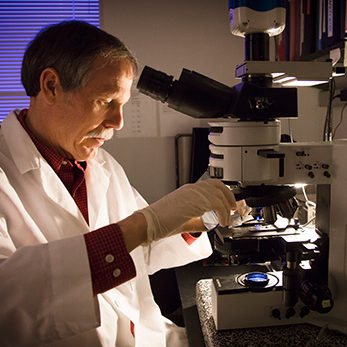
Our grantee Dr. Mario Buffone has been working in the field of sperm physiology for two decades. His lab seeks to understand the complex process of mammalian sperm capacitation, the change sperm undergo in the female reproductive tract that enables them to penetrate and fertilize an egg.
Dr. Buffone is working to screen and identify drugs that are able to prevent the capacitation and therefore render sperm incapable of fertilizing an egg. MCI is supporting the Buffone lab’s studies with the intent of moving towards in vivo preclinical studies. |
A biodegradable implant injected just below the skin’s surface that can deliver a male contraceptive over a sustained period of time.
|
Our grantee Dr. Rahima Benhabbour designs and fabricates delivery platforms for HIV prevention, cancer treatment, and contraception.
Dr. Benhabbour launched her first start-up AnelleO, Inc. in 2016, focusing on developing 3D-printed intravaginal rings for the treatment of infertility. MCI’s support will help facilitate studies that develop and implement an injectable device that can carry drug and translate into human studies. |
A daily, or even on-demand, method of male birth control that prevent sperm from being able to swim when taken.
|
Our grantee Dr. Gunda Georg’s group has published over 200 scientific articles on the design, synthesis, and evaluation of biologically active agents. In addition to male contraception, her lab investigates areas of cancer and female contraception.
Dr. Georg's lab has focused on investigating the testis-specific serine kinase (TSSK) family. These proteins are expressed after sperm have been developed, and are likely involved in multiple steps that could make them excellent contraceptive targets. MCI’s support will help Dr. Georg’s team investigate the sperm-specific isoform of Na,K-ATPase, which is crucial for sperm motility (e.g., sperm’s ability to swim). |
|
Our grantee Dr. Mike O’Rand is the President and Chief Scientific Officer of Eppin Pharma, named after the protein EPPIN which is a critical component of sperm development.
Dr. O’Rand is developing a compound called EP055, a small organic compound that that targets EPPIN on the surface of sperm and prevents sperm from swimming. MCI’s support will help support Dr. O’Rand Investigational New Drug (IND)-enabling milestones that are required for Eppin Pharma to begin the process of entering first-in-man studies for EP055. |
A reversible male birth control method that causes sperm to become sterile.
|
Our grantee Dr. Stephen L’Hernault and his lab have worked on spermatogenesis (i.e., sperm creation) and fertilization for over 30 years.
Dr. L’Hernault is working on developing compounds that can block the function of the IZUMO1 protein, which is required to fertilize an egg. MCI’s support will help Dr. L’Hernault’s team to identify small compounds that reversibly block the function of the IZUMO1 protein. |
A cohort of excited young researchers motivated by curiosity, ambition, and the social good associated with male birth control.
|
Our Fellowship program features a mix of graduate and postdoctoral trainees, all working towards creating non-hormonal, reversible male contraceptive methods.
Our Fellows work on a diverse portfolio of projects that help move the male birth control forward. Our support allows our distinguished Fellows to focus on the research, publish data, and build the background they need to sustain a long career as an investigator. |
An on-demand method of male birth control that you take just before sex.
|
Drs. Lonny Levin and Jochen Buck are professors at Weill Cornell Medicine and are working on inhibitors of soluble adenylyl cyclase (sAC) as on-demand male contraceptives. Their deep expertise in sAC keeps them attuned to the effects of inhibitors on sperm functions such as motility.
MCI is supporting work that develops novel inhibitors of sAC as on-demand male contraceptives as well as translational research that assesses the pharmacodynamics of inhibitors on human sperm. These steps are crucial to understanding how the drug stays associated to sperm after ejaculation and its potential contraceptive efficacy. |
Get Involved
Your support is vital to advancing male contraceptive research and empowering reproductive autonomy for all. There are several impactful ways you can make a difference:
|
Donate
It can cost over 1 billion dollars to bring a new contraceptive to market, so your financial contribution directly fuels the development of innovative male birth control alternatives. |
|
Spread Awareness
You can play a significant role through advocacy efforts. Start conversations with friends or family about the importance of shared family planning responsibility. Share our webpage, infographics, videos, or other resources among your networks to educate others. |
|
Volunteer
As a small team, we welcome volunteers who are passionate about driving change. You might be interested in joining one of our youth initiatives, or taking a survey to share your perspective on male birth control. If you're interested in lending your skills, time, or expertise, please contact us! |
Your contribution, whether through donations, spreading awareness, or volunteering, strengthens our collective efforts to reshape family planning and create a future where diverse male contraceptive options are accessible to all. Join us in advocating for reproductive autonomy and playing a role in shaping a more inclusive and equitable world.
MCI's "Advocating for Male Contraception" Animated Video
Frequently Asked Questions (FAQs)
About us
Male Contraceptive Initiative (MCI) is a 501(c)3 nonprofit whose objective is to advocate for and promote the development of reversible non-hormonal male contraception. MCI was founded in 2014 by a group of interested individuals who saw a philanthropic model as an innovative method to promote the development of male contraceptives. Since then, we have grown in scope and capacity, funding over $5M in research activities since our inception. Our Executive Board comprises experts in medicine, research, contraceptive development, and marketing, and we retain key advisors and stakeholders in the contraceptive research space.
MCI’s vision is “Reproductive Autonomy for All” and our mission is “To empower men, and couples, to fully contribute to family planning goals by providing them the resources they need for reproductive autonomy.”
We fund scientific studies, support early-stage researchers, and engage with the public on why male contraception will yield an advanced and as yet, unimagined modern landscape that:
We are funded through private donations from people like you. Join us on our journey to make “Reproductive Autonomy for All” a reality!
MCI’s vision is “Reproductive Autonomy for All” and our mission is “To empower men, and couples, to fully contribute to family planning goals by providing them the resources they need for reproductive autonomy.”
We fund scientific studies, support early-stage researchers, and engage with the public on why male contraception will yield an advanced and as yet, unimagined modern landscape that:
- Provides men with an option that is safe and reversible;
- Increases access and contraceptive choices for all;
- Enables informed choice about family growth and planning;
- Offers a complete menu of options for contraception;
- Fosters shared responsibility between spouses and partners;
- Reduces stress on the climate and environment; and
- Provides a solution for a heretofore unaddressed need
We are funded through private donations from people like you. Join us on our journey to make “Reproductive Autonomy for All” a reality!
What sort of products are in development?
Male contraceptives of the future can take a number of forms, with a wide range of product characteristics. This could be a daily pill, an implant, or even a coitally-dependent method that is taken only just before sex.
We like to think of male contraceptives in development as coming in three categories.
We like to think of male contraceptives in development as coming in three categories.
- Vas-occlusive devices. These can be likened to a vasectomy, and block the passage of sperm through the vas deferens. Unlike a vasectomy, these devices are intended to be reversible, and act long-term.
- Drug-based non-hormonal male contraception. This area is a very broad topic, and includes multiple targets with multiple mechanisms of action. Products could take the form of pills, implants, gels, or other modes of delivery. Depending on a number of factors, non-hormonal male contraceptives could potentially be short-acting, or quite long-acting, and there are many projects in development that span these diverse potential product characteristics. MCI focuses our funds on methods like vas-occlusive devices and drug-based non-hormonal approaches.
- Hormonal male contraception. This method uses administration of exogenous hormones to shut down sperm production, and is in active development with governmental and other support.
When will it hit the market?
Science has intended to get male contraceptives on the market for decades. Of the products currently in development, current estimates are 15-20 years away for a drug-based product and 5-10 years away for a device.
Listen to Intended, a new podcast from us where we discuss male contraception--learning from the past, talking to the researchers of the present, and the users of the future.
Listen to Intended, a new podcast from us where we discuss male contraception--learning from the past, talking to the researchers of the present, and the users of the future.
Why do you only support non-hormonal efforts?
Hormonal male contraceptives are currently in clinical trials, with support from the NIH and other funders. Non-hormonal male contraceptives are comparatively underfunded, despite offering a greater opportunity for innovation and methods that meet the needs of more users. MCI supports non-hormonal, early-stage research efforts, investing in the long-term to create an eventual menu of options for men and women that meet their lifestyle and individual needs. We believe that all methods of contraception are meaningful components of a continuum of reproductive care necessary to provide everyone with the autonomy to decide what’s best for them and when.
What happens with the research you fund?
MCI strives for transparency in all our efforts. Our grantees publish their results as Open Access so that the broader community can learn about the latest advances in male contraception. Consistent with our global mission, we also promote access to the eventual products for communities worldwide.
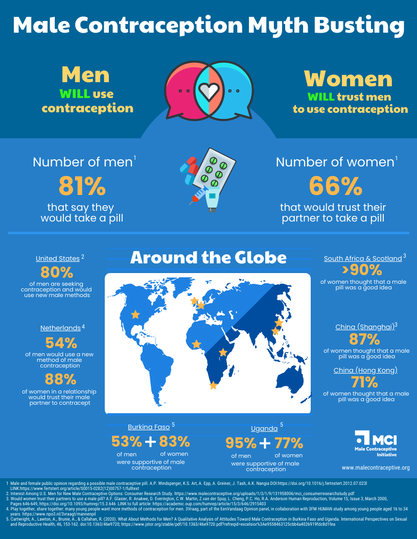
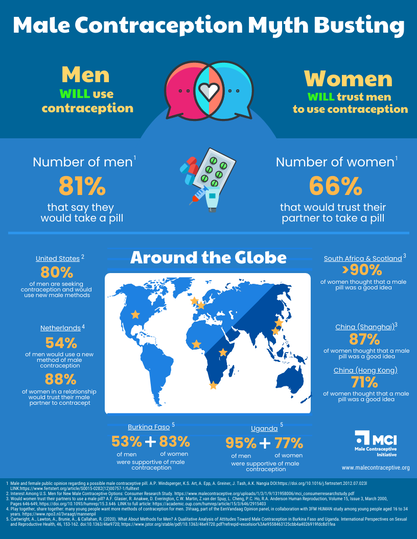
Will men actually use it?
|
There are multiple studies that show the majority of men are interested in male contraceptives, and want the ability to use them. MCI’s own research suggests a potential market of 17 million men in the United States alone. And that’s now – before there are any methods on the market at all. Once it becomes a normal conversation for men to be involved in contraception, we expect that more and more men will be interested.
|
Male Contraception Myth Busting
|
Will women trust men to use it?
|
Male contraceptives will allow new options for couples who find the current landscape doesn’t meet their needs. In surveys, most women would trust their partner to use male contraceptives. Male contraceptives will add to the method mix, providing new options that allow men and women to contribute in whatever way they deem appropriate to contraceptive use. Those who wish to continue using current forms of contraception will still have that option, and each situation will be unique to the individual.
|
Male Contraception Myth Busting
|
Why has it taken so long?
|
The unfortunate saying goes – “Male contraception has been 10 years away for the past 50 years.” There are many reasons for these delays including scientific hurdles, financing, and public interest. However, the field is more exciting than it’s ever been. Research is progressing down previously unexplored pathways with new technological advances, and an increasingly vocal contingent of men and women are highlighting the need for new options.
Our podcast Intended investigates the past, present, and future of male contraception. Season 1 is currently available and its episodes provide details as to why we don’t yet have contraceptive methods for men beyond the condom and vasectomy. |
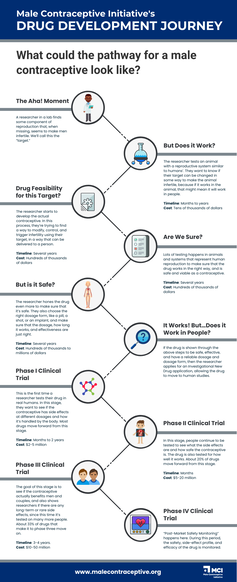
Drug Development Pathway
|
What are the biggest hurdles to making a male contraceptive?
First and foremost, funding. It can cost well over a billion dollars to get a drug all the way onto the market, and in an age where funding is scarce, male contraception rarely makes it to the top of the priority list. MCI pushes projects further along the pipeline to de-risk them and provide incentive for other funders to participate in the landscape.
Secondly, the regulatory pathway for male contraceptives is uncertain. These products will be unlike any other, and the steps required to ensure their safety and efficacy are yet-to-be determined. Male Contraceptive Initiative works with researchers and other stakeholders to clarify that regulatory path, and ask the important questions early. Other hurdles include the scientific challenges inherent in making a safe, reversible contraceptive that meets high clinical standards, and eventual policy issues in making it available for the consumer.
Secondly, the regulatory pathway for male contraceptives is uncertain. These products will be unlike any other, and the steps required to ensure their safety and efficacy are yet-to-be determined. Male Contraceptive Initiative works with researchers and other stakeholders to clarify that regulatory path, and ask the important questions early. Other hurdles include the scientific challenges inherent in making a safe, reversible contraceptive that meets high clinical standards, and eventual policy issues in making it available for the consumer.
What do you think about hormonal male contraception?
We’re very optimistic about hormonal male contraceptive trials, as they will allow men to participate in the family planning process in a way they haven’t been able to before. These eventual products will also create data about what men use, need, and enjoy about contraception, and shape how we guide the innovative products of the future.
Will male contraceptives offer STI / STD prevention?
Simply due to technology, first-generation male contraceptive products aren’t expected to offer sexually-transmitted infection / disease (STI) prevention. Multipurpose prevention technology (MPT) products are a class of products currently being researched to deliver contraception and varied combinations of HIV prevention and other STI prevention. We’re hopeful that innovative future products for men and women will find ways to incorporate these features.
Will women continue using their own contraception?
Many women use hormonal contraception for reasons other than preventing pregnancy. This is an individual choice for women to make on a case-by-case basis, considering their contraceptive needs, relationship, and other factors. We view contraception not as an “either, or” situation, but rather an “and” one: everyone should have access to the contraceptive methods they want and need. It is to everyone’s benefit that people have the tools and resources necessary to achieve their reproductive autonomy.
What are the differences between creating male and female methods?
|
There are lots of differences between developing male and female contraceptive options. Existing female contraceptives generally rely on using active pharmaceutical ingredients (APIs) that have already been approved by the Food and Drug Administration (FDA). This makes their approval and release easier, since much more is known about the safety and efficacy of the drug. Male options are yet to be developed, especially non-hormonal contraceptives. These drugs will need to be fully tested and vetted before they are allowed on the market.
In addition, biology is quite different. Female hormonal contraceptives generally work by preventing ovulation, thickening cervical mucus, and thinning the lining of the uterus. Male contraceptives will need to target the creation or maturation of sperm, it’s transport out of the male reproductive system, or it’s ability to swim to and fertilize an egg. These drastically different biological functions are complex, and need in-depth scientific study to understand how we might block them in a targeted, non-systemic way. |
Existing Contraceptive Methods
|
How can I learn more about conferences and other events around the male contraception space?
We regularly update our Events page to provide you listings of local and international conferences and meetings. This page also gives you access to brief event descriptions along with logistical details. You can sign up for our newsletter to receive information on upcoming events.
Does Male Contraceptive Initiative have published works?
Male Contraceptive Initiative has completed several projects that have led to publication of scientific literature and in general media. Many of these studies and reports are self-published. We also highlight scientific articles that our grantees have published. These resources can be found on our Publications page.
Is there a place where scientific terminology and/or phrases are defined and explained further?
The Glossary provides you quick access to a collection of defined scientific terms and phrases. It also includes words from popular culture in reference to the male reproductive system. You can also visit our videos and webinars, as well as our blog for more in depth explorations of these concepts and terminologies.
Where can I sign up?
You can sign up for our newsletter below for updates on MCI. We’ll notify you of new ways you can participate in the creation of methods for men as we have them.
Is vasectomy reversible?
While vasectomy is intended to be permanent, reversal procedures are available but not guaranteed to restore fertility. Consider this decision carefully if you're uncertain about future family plans.
Does vasectomy affect sexual function or desire?
Vasectomy doesn't affect libido or sexual function. It only prevents the release of sperm during ejaculation. Sexual pleasure remains unchanged.
Is the vasectomy procedure painful?
|
Vasectomy is an outpatient procedure, usually done under local anesthesia, minimizing discomfort. Mild soreness might follow, but it's temporary.
|
MCI's "Nuts & Bolts: 10 Facts About Vasectomy" Animated Short
|
Do condoms provide protection against STIs?
Yes, condoms offer dual protection by preventing both unwanted pregnancies and sexually transmitted infections.
How effective at preventing pregnancy are condoms?
With “perfect use”, the effectiveness rate can be as high as 98%. The “typical use” effectiveness rate is usually somewhere between 82-90%. This means that couples relying solely on condoms for birth control can experience a pregnancy as often as once every five times they have sex.
Check the expiration date, handle with care, and ensure proper fit for proper efficacy.
Check the expiration date, handle with care, and ensure proper fit for proper efficacy.