Everyone on the gender spectrum deserves to have reproductive autonomy. We are working towards a world where everyone has access to sexual and reproductive health products and, therefore, more control over their family planning goals.
Key Points/Learning Objectives
- How is gender identity impacted by male contraception?
- How can male contraception empower the LBBTQ+ community?
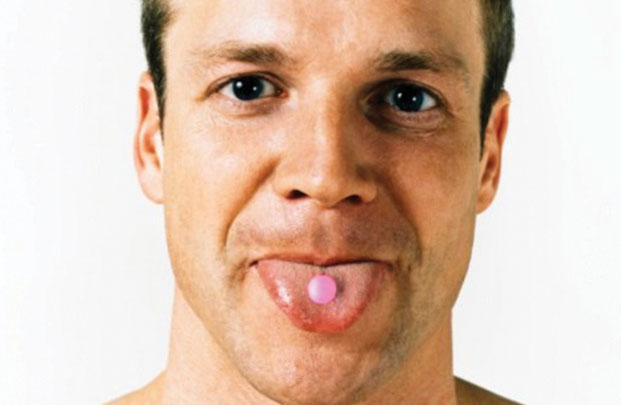
Modern hormonal and prescription contraception is primarily focused on giving cisgender women, or people who identify as women who were also assigned female at birth, the means to protect themselves against an unintended pregnancy. While pills, patches, and IUDs are useful tools to help cis women control their fertility, they may fall short at protecting some cis men, trans, nonbinary, and intersex people. In recent years, there has been an increased awareness of sexual and reproductive health disparities adversely affecting LGBTQ populations.
Reproductive Autonomy For All
At MCI, we believe that our work is more than just drug or product development. It's a mission to empower everyone with the freedom to choose how they manage their fertility, contraception, and family planning.
We want people across the gender and sexuality spectrum to benefit from the contraceptive methods we support and advocate for. Because of the systemic and limited views of gender identity and sexual orientation, we overlook marginalized groups in product development and research for contraception.
The focus has been on ciswomen as child-bearers and contraceptive users, limiting science and society. Every person deserves the freedom to choose if and when they want children. The responsibility of contraception should not fall solely on people who produce eggs.
If we want to reach true equality for everyone, we need to include everyone in the critical conversations. When it comes to reproductive education for those outside the cis-het (cisgender and heterosexual) system, most of us received close to nothing—leaving an entire group of people to fend for themselves.
We need health care to address the need for sperm targeting contraception. Socially we need to acknowledge that not everyone who produces sperm is a man.
We see that the binary system is limiting and exclusive. It is time for all people to be part of the contraceptive conversation.
We want people across the gender and sexuality spectrum to benefit from the contraceptive methods we support and advocate for. Because of the systemic and limited views of gender identity and sexual orientation, we overlook marginalized groups in product development and research for contraception.
The focus has been on ciswomen as child-bearers and contraceptive users, limiting science and society. Every person deserves the freedom to choose if and when they want children. The responsibility of contraception should not fall solely on people who produce eggs.
If we want to reach true equality for everyone, we need to include everyone in the critical conversations. When it comes to reproductive education for those outside the cis-het (cisgender and heterosexual) system, most of us received close to nothing—leaving an entire group of people to fend for themselves.
We need health care to address the need for sperm targeting contraception. Socially we need to acknowledge that not everyone who produces sperm is a man.
We see that the binary system is limiting and exclusive. It is time for all people to be part of the contraceptive conversation.
Sex and Gender
To understand "reproductive autonomy for all," it is vital to learn the difference between sex and gender. Cisgender people may have never realized there is a difference because their sex and gender align.
|
Sex (n): either of the two major forms of individuals that occur in many species and that are distinguished respectively as female or male, especially on the basis of their reproductive organs and structures. (source)
|
Gender identity (n): a person's internal sense of being male, female, some combination of male and female, or neither male nor female. (source)
|
While many experiences no difference between their sex and gender identity, sex and gender identity variations are vast. But for those who do experience gender differences, it can be a confusing and long journey. Gender dysphoria is a genuine and often very intense feeling, where how you look outside, doesn't match how you feel inside. For many people outside the gender binary, gender dysphoria is common.
Due to the many variations of sexuality, equal access to a variety of contraception is necessary.
Investigating the LGBTQ+ Community’s Contraceptive Needs
This blog post is by Brittany Chambers, a 2020 MCI intern from North Carolina Central University. Read how she used field testing to gain insight into how to develop a survey tool used to develop methods that take into account the needs of LGBTQ+ individuals.
At MCI, we work to advance a wide range of technologies that span the gamut, and focus on the end goal of meeting the needs of as many users as possible across the time in which they choose to contracept. We do this by understanding the biological significance of specific contraceptive targets, then extrapolating to determine what types of products could result from contraceptives that exploit them. Pills, injectables, on-demand methods, and long-acting methods are all a part of our portfolio and part of how we move towards a world with true contraceptive choice.
Developing Contraceptives for All Users
Transmasculine Individuals
\s society’s relationship with gender and sexuality evolves, the way that we think about preventative healthcare services should evolve as well. In order for health care to better serve transmasculine people, it is important to prioritize individualization of care to cater to the needs of each client.
The challenge is that society, up until now, has looked at health care, sexuality, and reproduction through a binary lens. Fertility services and contraceptive options have mostly been geared towards helping (cis) women prevent instances of unintended pregnancy or plan future pregnancies. If cis men lack the resources to meaningfully contribute to family planning goals due to limited methods, what chance does anybody else have? If the healthcare system can find ways to de-gender health services and contraception, then reproductive health services will become more accessible to not only cis men, but also trans, intersex, and nonbinary individuals.
The challenge is that society, up until now, has looked at health care, sexuality, and reproduction through a binary lens. Fertility services and contraceptive options have mostly been geared towards helping (cis) women prevent instances of unintended pregnancy or plan future pregnancies. If cis men lack the resources to meaningfully contribute to family planning goals due to limited methods, what chance does anybody else have? If the healthcare system can find ways to de-gender health services and contraception, then reproductive health services will become more accessible to not only cis men, but also trans, intersex, and nonbinary individuals.
Reproductive Autonomy for Transmasculine Individuals
This study conducted an exploratory study to understand current contraceptive practices and fertility desires among transgender men during and after transitioning.
"Family planning and contraception use in transgender men" by Alexis Light, Lin-Fan Wang, Alexander Zeymo, and Veronica Gomez-Lobo
This research examines contraceptive methods used by adolescent/young adult women of diverse sexual orientations.
“Sexual orientation-related differences in contraceptive use: A brief report based on a cohort of adolescent and young women” by Brittany M. Charlton, Colleen A. Reynolds, Elizabeth Janiak, Amy D. DiVasta, Rachel K. Jones, Jorge E. Chavarro, Vishnudas Sarda, S. Bryn Austin
"Family planning and contraception use in transgender men" by Alexis Light, Lin-Fan Wang, Alexander Zeymo, and Veronica Gomez-Lobo
This research examines contraceptive methods used by adolescent/young adult women of diverse sexual orientations.
“Sexual orientation-related differences in contraceptive use: A brief report based on a cohort of adolescent and young women” by Brittany M. Charlton, Colleen A. Reynolds, Elizabeth Janiak, Amy D. DiVasta, Rachel K. Jones, Jorge E. Chavarro, Vishnudas Sarda, S. Bryn Austin
Transfeminine Individuals
Nuts & Bolts: Transfeminine
Typically, society views sexual and reproductive health (SRH) services through a heteronormative gender binary lens, where protecting cisgender women from unintended pregnancies is the main focus.Nonbinary and transgender people are often left out of the greater conversation around sexual and reproductive health, including contraception.
There is a lack of awareness and sex education about LGBTQIA+ people and methods of birth control or general reproductive health. This means many people in this community have to fend for themselves or rely on potentially dangerous information.
There is a lack of awareness and sex education about LGBTQIA+ people and methods of birth control or general reproductive health. This means many people in this community have to fend for themselves or rely on potentially dangerous information.
- For example, a common misconception is that gender-affirming hormones can serve as an effective method to prevent pregnancy for everyone. However, transfeminine people who produce sperm are still at risk of causing an unintended pregnancy with their partner if they rely on these methods.
Reproductive Autonomy for Transfeminine Individuals