Current contraception options available for men are falling short because there is no long-term male birth control option. Vasectomies are perceived as an irreversible method, and the real-world pregnancy rate for the condom is 13% – a truly high number if you’re looking for a fail-safe birth control method.
Key Points/Learning Objectives
- Current developing and new ideas for male contraceptive methods that we are expecting in the near future
- Resources and funding for future male contraception
The Future of Male Contraception
Better contraceptive options for men will bring equity to family planning, as more men share the fertility responsibility.
Every new female contraceptive method created has resulted in increased contraceptive use, fewer unintended pregnancies, and healthier children around the world. We expect the same to be true for future developments in new male contraception.
It’s imperative we make a push for male birth control today. There are 80 million unintended pregnancies each year worldwide. There hasn’t been significant innovation in contraception, particularly non-hormonal methods, for decades.
Reducing unintended pregnancies can help break the cycle of poverty. Researchers also expect to save taxpayers over $5 billion per year in short-term medical costs. Savings in long-term costs are expected to be much larger, just by ensuring family planning needs are met for all.
Every new female contraceptive method created has resulted in increased contraceptive use, fewer unintended pregnancies, and healthier children around the world. We expect the same to be true for future developments in new male contraception.
It’s imperative we make a push for male birth control today. There are 80 million unintended pregnancies each year worldwide. There hasn’t been significant innovation in contraception, particularly non-hormonal methods, for decades.
Reducing unintended pregnancies can help break the cycle of poverty. Researchers also expect to save taxpayers over $5 billion per year in short-term medical costs. Savings in long-term costs are expected to be much larger, just by ensuring family planning needs are met for all.
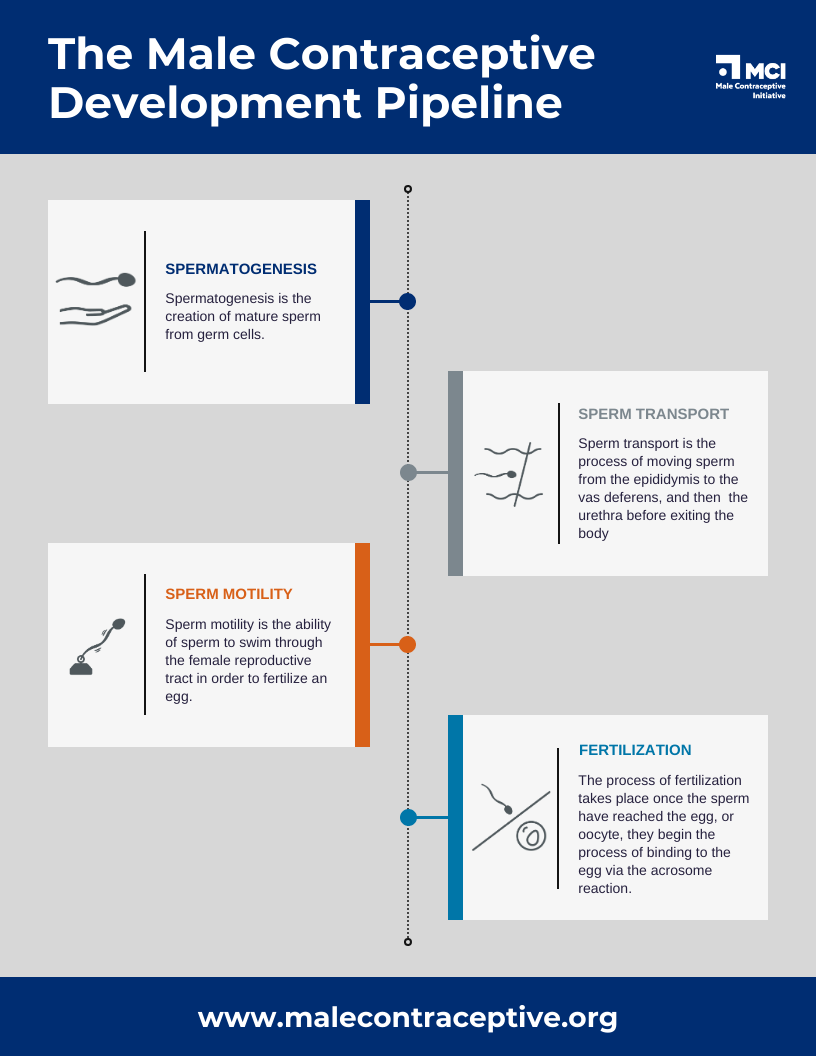
Nuts & Bolts: The “Male Pill”
In this episode, we provide a brief explanation of what the "Male Pill" could look like, and why there is cause for excitement about the future of male birth control.
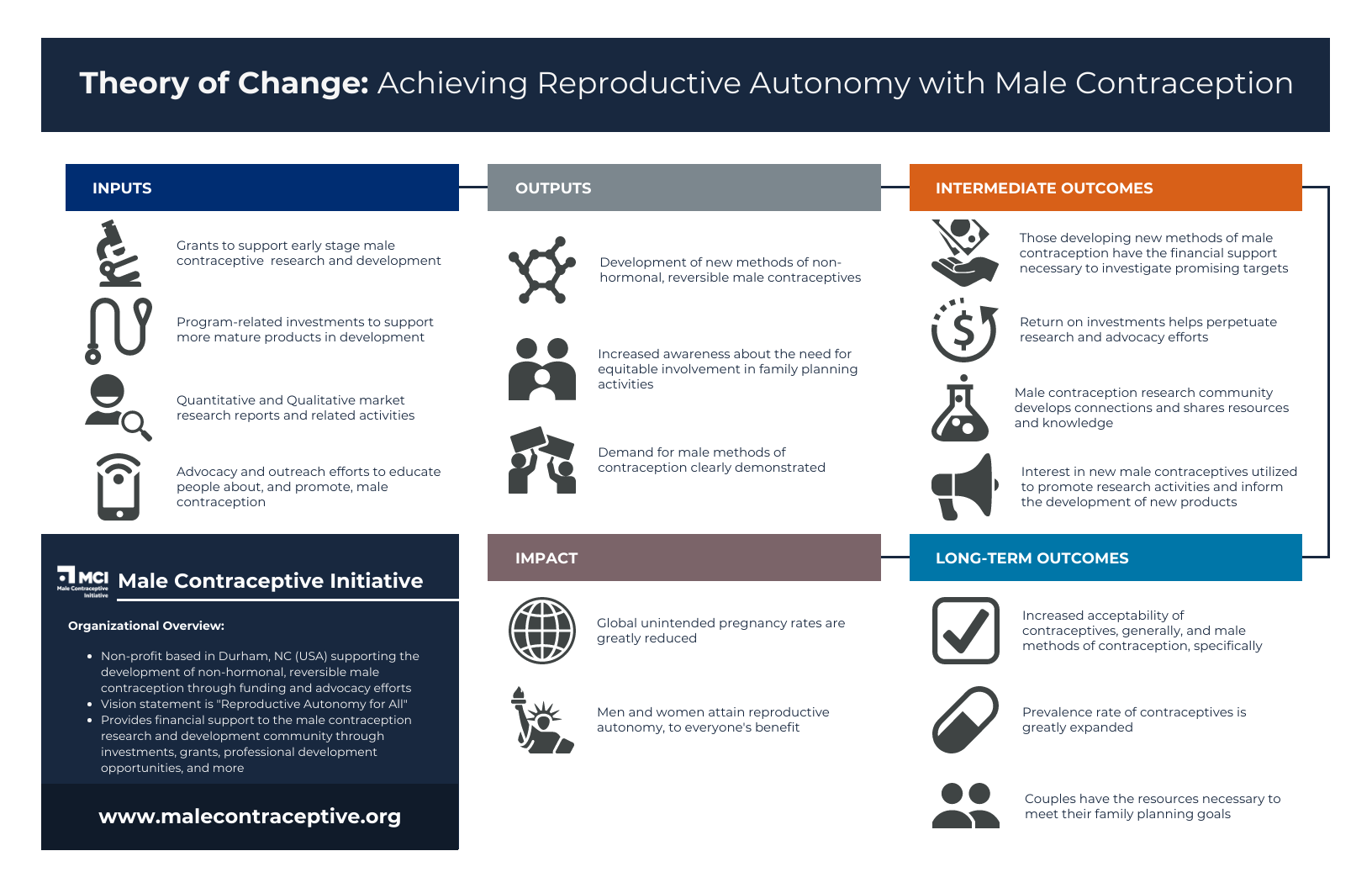
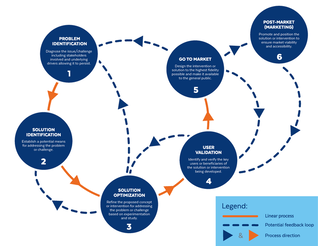
Male Contraceptive Initiative’s Theory of Change
In this short animated film, we provide an overview of our Theory of Change: achieving reproductive autonomy for everyone through increased methods of male birth control.
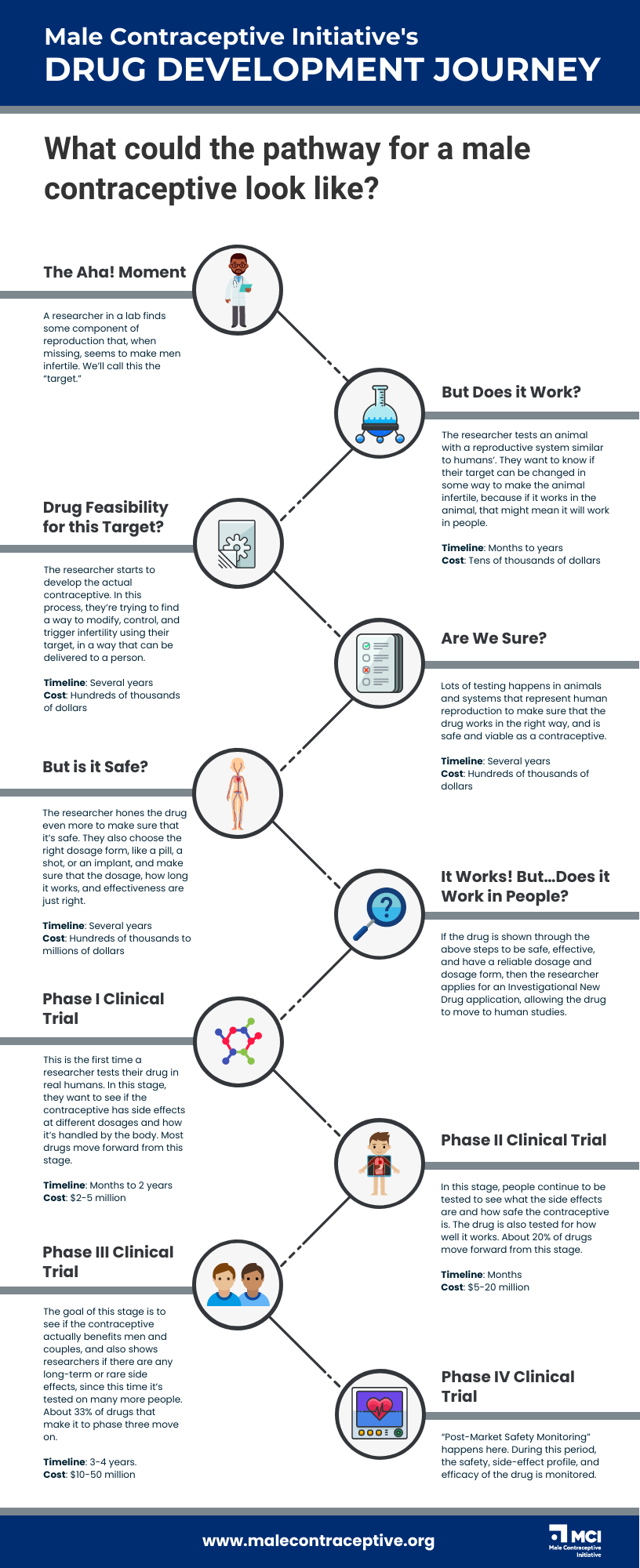
Drug Development
What potential male contraceptives are out there, and when will they be available?
MCI’s NHRMC Target Database
The Drug Development Pipeline, Simplified
Read this post to learn about the ways that a drug makes it to market and why male contraceptives are still in development.
Funding Drug Development
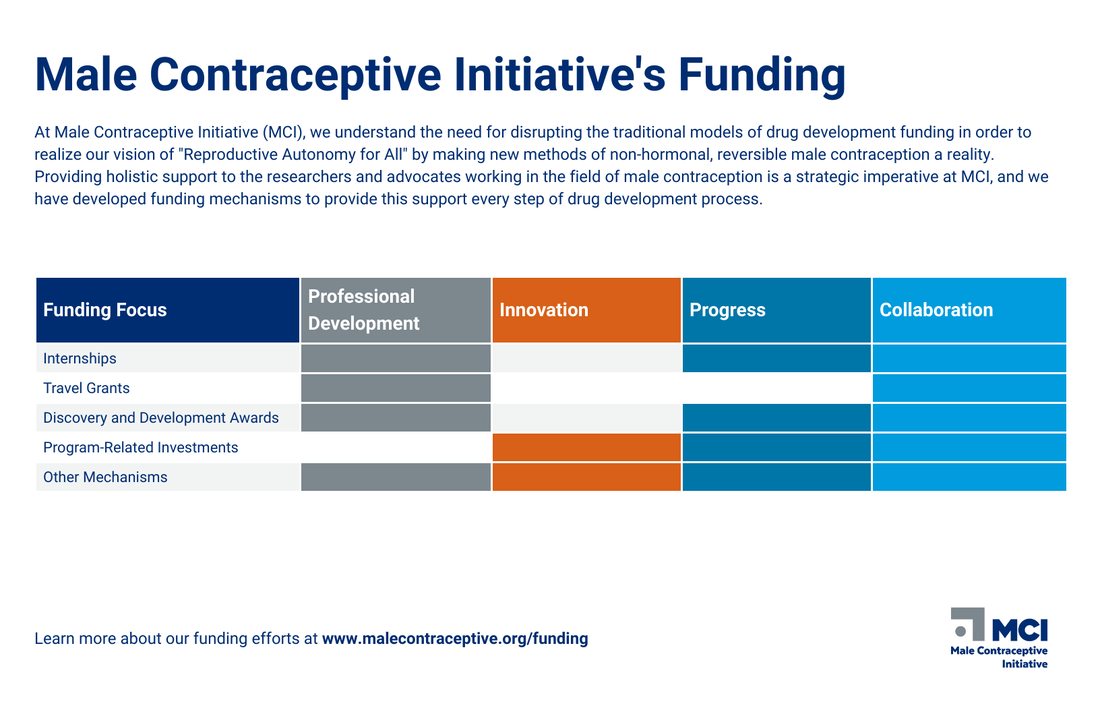
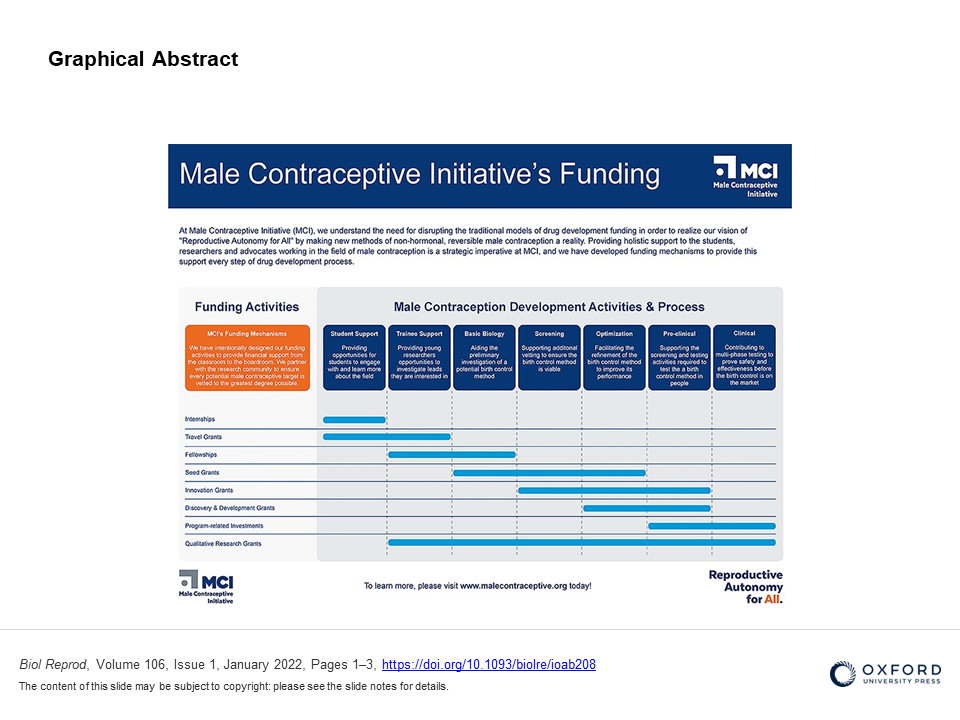
Male Contraceptive Initiative’s mission is, “to empower men, and couples, to fully contribute to family planning goals by providing them the resources they need for reproductive autonomy.” It is how we articulate our most hopeful vision of the future: one where there is reproductive autonomy for all people. This vision and associated mission directs our daily activities, which encompass financial support to the male contraception research community and advocating for the development of additional male contraceptives.
Funding the Next Contraception Revolution
MCI's Funding Strategy
In this short animated film, we simplify and elucidate the funding sources for contraceptive research and development, illustrating the critical role that philanthropic sources like MCI play in ensuring innovation in the sector.
This Forum outlines the purpose of and funding opportunities provided by Male Contraceptive Initiative, a funding agency and non-profit focused on the advancement of non-hormonal, reversible contraceptive technologies for those who produce sperm.
Clinical Trials, Simplified
In this short animated film, we attempt to simplify the clinical trial process in an effort to illustrate the steps necessary to get a new contraceptive or drug to market.
Each year, there are over 120 million unintended pregnancies experienced around the world, while the global population increases by over 80 million people. This constant human population growth has already translated to multiple significant challenges around the world, and will continue contributing to increased ecological degradation, conflict, climate change, natural disasters, global pandemics, and more. It is a reality that negatively impacts all of us. Consider this: unintended teen pregnancies in the United States are estimated to cost American taxpayers over $9 billion annually.
Increasing access to contraception in order to meet existing unmet needs in low- and middle- income countries alone would lead to a 68% reduction in unintended pregnancies; there are over 200 million women in these contexts actively seeking more and better methods.
When considering men, the birth control situation is even more dire as there are currently only two methods of contraception available to sperm-producers: condoms and vasectomy. Lack of acknowledgement of this inequity and the need for additional male-controlled methods persists despite demonstrated demand for more methods (with an estimated 17 million men in just the United States with unmet family planning needs) and over 60 years of research and development efforts.
Bringing a new drug to market is not easy, and it is very expensive: the estimated median capitalized research and development cost per product is nearly $1 billion. In most situations these costs are incurred by large pharmaceutical companies who then recoup these costs in the pricing of their products. However, most contraceptive products are not developed by pharmaceutical companies, rather the development is heavily subsidized by non-profit and government agencies. Given the layered challenges that contraceptive product development faces, It is imperative that researchers, advocates, and the general public support organizations like Male Contraceptive Initiative if we are to make male contraception a reality.
Increasing access to contraception in order to meet existing unmet needs in low- and middle- income countries alone would lead to a 68% reduction in unintended pregnancies; there are over 200 million women in these contexts actively seeking more and better methods.
When considering men, the birth control situation is even more dire as there are currently only two methods of contraception available to sperm-producers: condoms and vasectomy. Lack of acknowledgement of this inequity and the need for additional male-controlled methods persists despite demonstrated demand for more methods (with an estimated 17 million men in just the United States with unmet family planning needs) and over 60 years of research and development efforts.
Bringing a new drug to market is not easy, and it is very expensive: the estimated median capitalized research and development cost per product is nearly $1 billion. In most situations these costs are incurred by large pharmaceutical companies who then recoup these costs in the pricing of their products. However, most contraceptive products are not developed by pharmaceutical companies, rather the development is heavily subsidized by non-profit and government agencies. Given the layered challenges that contraceptive product development faces, It is imperative that researchers, advocates, and the general public support organizations like Male Contraceptive Initiative if we are to make male contraception a reality.
MCI Grantees
|
Dr. Patricia S. Cuasnicu is a Senior Scientific Researcher from the National Research Council (CONICET) at Argentina’s Instituto de Biologia y Medicina Experimental (IBYME-CONICET) in Buenos Aires. MCI awarded Dr. Cuasnicu with a $150,000 seed grant in 2018 to aid in the continuation of her work.
|
Ed Gillis is the CEO of Revolution Contraceptives. The company is currently working on Vasalgel, a device being developed as a long-acting, non-hormonal contraceptive intended to be reversible. He is an entrepreneur and senior level executive with proven success in early and mid-stage fundraising, OUS clinical trials, research and development and clinical manufacturing of products in early stage companies.
|
|
Dr. Wei Yan is University of Nevada, Reno Foundation Professor and Director of Single Cell Genomics & Genome Editing Core Labs at the University of Nevada, Reno School of Medicine. His lab works on genetics and epigenetics of gametogenesis, and epigenetic contribution of gametes to fertilization, early embryonic development and adulthood health.
|
Dr. Sab Ventura teaches undergraduate Pharmacy and Pharmaceutical Science students and is the Head of the Male Reproductive Pharmacology Research Lab. He has co-authored 79 peer reviewed publications and his research investigates the physiology and pharmacology of male reproductive organs with a view to identifying novel therapeutic targets for male contraception.
|
Challenges Surrounding Male Contraception Development
|
Why Male Birth Control Is So Hard To Make
|
MCI's Lemonade Stand: "Common Challenges in Formulation Development for Long-Acting Products"
|
Survey
Survey: Ideal Male Contraceptive Methods